Have I ever paused to consider what truly unfolds when blood flow suddenly stops reaching one side of my sight? It may sound small at first, yet when a clot settles inside a narrow channel carrying oxygen-rich blood, everything can shift in an instant. Without that steady stream, vision can blur, dim, or disappear almost immediately. Why does change strike so quickly? Because sight links directly to brain tissue, and even a brief interruption can disturb what I’m able to process. Picture a home during a blackout—lights flicker out, screens go dark, routines come to a halt. That same rapid shift can occur within moments. And here’s a powerful truth: recognizing those sudden changes right away can shape what happens next in a meaningful way.
Eye Stroke Causes, Symptoms, and Prevention Tips
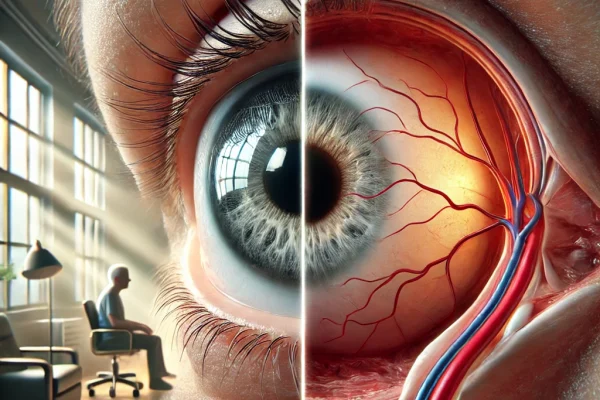
Let’s dive into a subject often overlooked yet deeply significant—vision-endangering emergencies. Circulation disturbances that influence brain function can also extend their reach to eyesight, disrupting clarity and focus in unexpected ways. Such incidents may trigger abrupt changes, sometimes occurring within moments, leaving a person startled and anxious. Early recognition of those warning signs can mark the difference between saving vision and facing long-term impairment. So, grab a warm cup of coffee, settle into a comfortable spot, and explore essential insights surrounding these sudden, sight-altering conditions.
What Is an Eye Stroke?
There are two main types of these strokes affecting vision:
Central Retinal Artery Occlusion (CRAO):
This condition develops when a vital channel supplying nourishment to a central zone responsible for detecting light and shapes becomes restricted or completely blocked. That pathway works like a lifeline, carrying oxygen and essential nutrients required to maintain smooth visual processing. Once that flow gets interrupted, cells in that area start struggling, leading to blurriness, distortion, or even vision loss as image clarity fades away.
Picture a vast city built around one main highway. Every truck carrying goods, every courier delivering packages, every emergency vehicle rushing toward its destination depends on that single stretch of road. Now imagine that route suddenly blocked. Chaos doesn’t strike right away, yet small disruptions start to spread. Stores wait for shipments that never arrive, groceries sit empty, and responders face long delays. Bit by bit, routines crumble, traffic snarls grow worse, and daily life slips out of rhythm. Slowly, what once ran smoothly turns into confusion and frustration across the entire city.
That’s exactly how CRAO unfolds. When that primary inner pathway narrows or becomes blocked, delicate tissue inside begins to struggle almost immediately. Can this process be seen from outside? No. Does invisibility make it any less serious? Absolutely not. That fragile layer gathers every detail relied upon each day—light, shadow, color, shape, depth—and delivers those signals directly to brain centers responsible for perception. When that flow is interrupted, those messages weaken or stop, and clarity can fade in a matter of moments.
So when supply weakens, what happens next? Clarity begins to slip. Fine details lose their sharp edge. Something feels different, almost unsettling. Is that subtle change worth attention? Absolutely. That quiet shift can signal something far more significant unfolding beneath surface awareness. Here’s a truth that deserves confidence: recognizing that change early can safeguard what matters most. Brushing it aside may feel easier in moment, yet tuning in to instinct reflects wisdom, not fear. Awareness is strength, and swift recognition can influence what comes next in a powerful way.
Without prompt intervention, affected tissue starts deteriorating rapidly, disrupting normal communication within a brain. Signals from that area struggle to pass through, leading to a sharp drop in coordination and awareness. With no alternate route to reroute information, damage escalates quickly, making recovery much harder. It resembles a city plunged into darkness during a power outage—without a backup generator, every function stops until immediate measures restore flow.
This situation carries far greater seriousness than issues occurring in smaller passageways since it affects a major route responsible for essential flow. Once this central pathway becomes obstructed, movement ceases entirely, preventing anything from reaching its destination. That’s why CRAO often leads to far more severe outcomes compared to blockages in secondary or smaller vessels.
Branch Retinal Artery Occlusion (BRAO):
What happens when a tiny pathway that feeds sight suddenly closes without warning? At first, there may be no pain—just a subtle shift. Doesn’t that quiet change feel unsettling? Picture a lively Canadian town where highways remain open and traffic flows smoothly, yet one small side street becomes blocked. Homes at end of that road stop receiving deliveries. From a distance, everything appears normal. Streets stay busy. Lights remain on. Life carries forward. But something essential is missing, isn’t it? That silent disruption matters more than it seems. When clarity fades without noise or drama, instinct often senses truth before logic does. Listening to that inner signal isn’t overreaction—it reflects awareness and strength.
That’s exactly how this issue unfolds. A small branch that once carried oxygen and vital nutrients toward sight centers inside skull becomes restricted, and even though main routes may still flow, doubt can creep in—“Is this serious? Will this pass?” Yet when part of vision begins fading, dimming, or warping, that moment carries meaning. Ignoring it may feel easier, but awareness creates strength. Swift response places control back where it belongs. Paying close attention guards what matters in profound ways. And here is certainty worth holding onto: early action truly can change outcome.
When this kind of narrowing begins, vital nutrients no longer travel as intended. Have I ever caught part of a scene looking dull, warped, or slightly shadowed and paused with a quiet thought—“Is something off?” That reaction isn’t imagination. Areas above, below, or along edges can appear hazy, as if fine details slipped away without notice. Why does that feel so unsettling? Because clarity shapes confidence, and when vision shifts, certainty can waver too. Ignoring it might feel convenient, yet awareness creates advantage. Recognizing those early distortions reflects strength, not fear. Taking that step promptly can influence what continues to be seen and experienced each day in meaningful ways.
Even if a main pathway remains active, a blockage or disruption in a smaller route can still interfere with signal transmission from certain areas to a brain. Everyday tasks like reading a sentence, navigating a familiar room, or recognizing a face can become confusing, especially when that disrupted channel is relied on for sensory input.
Intensity of this experience varies based on where disruption takes place. At times, it strikes without any hint, catching a person off guard. Pain might not always be present, yet perception of surroundings can feel distorted, giving a sense of imbalance that turns ordinary tasks into challenges.
Both conditions may bring about major sight challenges, yet CRAO often triggers a faster and more intense decline in clarity than BRAO. Keeping that in focus, let’s take a closer look at warning signals that may show up before or during such incidents, allowing early recognition and quick action.
Signs and Symptoms to Watch For
What makes these moments so deeply unsettling? It’s how quietly change slips in. No alarms, no dramatic warning—just a subtle shift that catches awareness off guard. One moment a scene appears clear and familiar, next moment part of it softens, blurs, or seems to vanish. Has that sudden distortion ever sparked a thought like, “What just happened?” That confusion carries meaning. Sudden visual change without explanation is not random noise—it’s information. Dismissing it may feel easier in moment, yet attentiveness creates protection. Even small, unusual differences deserve respect. Noticing early signals can stand between temporary disruption and something far more serious.
Ever experienced a moment when one side of vision begins to fade and a quiet thought surfaces—“Is this really happening?” Rubbing eyes, blinking, waiting… yet nothing sharpens. Colours appear washed out, edges soften, and a shadow drifts in like a curtain closing at mid-day. Could it simply be fatigue or long hours in front of a screen? That explanation feels comforting, doesn’t it? Yet instinct often whispers when something deeper is unfolding. Absence of pain does not equal absence of risk. That sudden dimming serves as a signal, not a coincidence. Why delay and gamble with further loss when swift movement creates possibility? Acting quickly restores a sense of control, and that timely response can safeguard what holds immense value each day.
Partial Vision Loss: Ever caught a portion of a scene simply… fading? Perhaps an upper corner looks dim, or a lower area turns shadowed or blank. It can resemble looking through glass marked by one stubborn cloudy patch that refuses to clear. A quiet question may surface—“Is this just fatigue, or something more?” When a section disappears without warning, unease makes perfect sense. Ordinary tasks—reading a few lines, walking across a room, stepping behind a wheel—can suddenly require sharper concentration. Why does such a subtle change feel so significant? Because even a small gap in vision alters how surroundings are understood. That kind of shift is not background noise. It serves as a signal. Noticing it, respecting it, and responding promptly can make a meaningful difference in what continues to be seen and experienced each day.
Has a gray or dim patch ever lingered in view, refusing to fade no matter how often blinking or shifting focus occurs? Rubbing eyes, looking away, returning again—yet that shadow stays. Frustrating, isn’t it? A quiet thought may rise: “Is this harmless… or a sign that deserves attention?” When reading demands more effort, faces lose sharp detail, or simple movement feels slightly uncertain, that persistent dimness is not random. Delicate brain tissue relies on steady, precise signals, and even a small disruption makes its presence known. Brushing it aside may seem easier, yet intuition often senses importance before logic forms clear answers. If that muted area continues to linger, respect becomes essential. Choosing action early reflects awareness and inner strength—and that timely decision can safeguard clarity for meaningful moments still ahead.
Altered Perception of Shapes and Sizes
Have you ever paused and wondered, Why does everything suddenly feel off? Do door frames appear to bend, pages seem uneven, or familiar objects look strangely smaller or stretched? Is it simple fatigue, or could something deeper be unfolding? When shapes twist and sizes shift without clear reason, that is not random imagination. That inner voice recognizes what feels normal and what does not, and when vision turns unfamiliar or unsettling, that reaction matters. Doubt may whisper that it is nothing, yet awareness answers with confidence—something has changed. Ignoring those moments rarely brings clarity, but acknowledging them shows courage. Real strength appears in that quiet decision to take changes seriously and move forward with intention.
Have tiny drifting dots or faint thread-like strands ever glided across vision, especially against a bright sky or plain wall, sparking that uneasy thought—“Is something wrong?” Take a steady breath. In many cases, these are simply Eye floaters, a common occurrence with natural aging changes inside the eye. As internal gel subtly shifts over time, small specks cast shadows that appear to float. Strange to see? Absolutely. Dangerous in most situations? No. Understanding this brings calm instead of fear. Knowledge replaces uncertainty with clarity, and clarity restores confidence. When awareness guides reaction, next steps feel steady, informed, and fully in control.
Have sudden bursts of floating specks, flashing lights, or a dark veil sweeping across vision ever sparked that urgent thought—“Why now?” That kind of shift can feel deeply unsettling, and brushing it aside rarely brings reassurance. When new flickers or shadows appear without warning, instinct often recognizes that something isn’t quite right. So why hesitate or second-guess that signal? Prompt medical evaluation can bring clarity, answers, and timely intervention if needed. Swift action is not panic—it reflects awareness, wisdom, and respect for vision. Choosing to respond quickly protects sight and preserves confidence for moments still ahead.
Discomfort or Tightness: While not everyone notices it, some people describe a gentle pulsing or mild tightness in one area. It may feel like a dull ache—an odd sensation that simply feels off. It isn’t sharp or severe, yet it’s noticeable enough to signal that something unusual is going on. This feeling often stays localized and may come with a sense of heaviness or strain, especially when trying to focus or stay alert. Although this isn’t a common early sign, it’s still worth paying attention to when it shows up suddenly without an obvious reason.
Why Does This Condition Happen?
Now that warning signs appear clearer, doesn’t curiosity naturally follow—what truly sets this process in motion? Fair question. Straight answer: disruption usually begins when steady blood flow carrying oxygen and vital nutrients to delicate light-sensing tissue becomes interrupted. What causes that break in movement? Often, it traces back to plaque buildup along artery walls—commonly linked to Atherosclerosis—or to a drifting clot that lodges where circulation must remain open. At times, persistently high glucose levels, as seen in Diabetes, gradually injure vessel linings and weaken those critical pathways. Unsettling? Certainly. Uncontrollable? Not at all. Understanding root causes creates leverage. With awareness comes opportunity to make informed decisions, reduce risk factors, and move forward with stronger protection and lasting confidence.
Clot Formation :
Inside exists a web of microscopic pathways meant to carry vital elements that sustain movement, feeling, and awareness. At times, these delicate routes face disruption when a dense cluster of cells, often called a clot, forms in an unusual spot. Such a cluster may arise right at an obstructed location or begin elsewhere, such as a large vessel along neck area or a central pumping organ. Once it breaks free, it moves through connected channels until reaching a narrow passage, where it becomes lodged, cutting off normal flow and disturbing usual function.
Imagine a bustling canal network delivering fresh water to small towns that depend on steady flow each day. What happens when debris drifts in and wedges tight within a narrow passage? Everything beyond that blockage begins to dry. Streets quiet down, fields crack, momentum fades. Now consider internal circulation—when a vital vessel becomes obstructed, oxygen and nutrients struggle to reach tissues relying on constant movement to remain strong. Without reliable flow, performance weakens and risk rises. Sound familiar? Early warning signs rarely shout, yet impact can be profound. Swift recognition and decisive action are not dramatic reactions; they are intelligent protection. Responding in time preserves strength, safeguards clarity, and keeps forward progress steady and uninterrupted.
Have subtle changes ever stirred a quiet question—“Is this only a passing moment?” Brushing it aside may feel easier, yet what if it lingers? When oxygen and vital nourishment fail to reach delicate tissues, resilience begins to weaken and responses may slow. At first, shifts seem minor, almost harmless. But can subtle warnings truly be ignored? Absolutely not. Persistent interruption can allow lasting injury to take hold, reshaping daily function in ways that grow harder to reverse. Awareness becomes power in that moment. Trusting instinct, acknowledging change, and choosing swift action reflect strength—not fear. Early response creates opportunity to protect what matters most and preserve clarity, capability, and forward momentum.
That’s why it’s crucial to be aware of what’s happening internally. While it may not always be possible to predict when or where a clot might lodge itself, understanding how it can affect sensitive structures gives us a better chance at minimizing long-term consequences through prompt and effective intervention.
Have questions ever surfaced about what quietly accumulates within arteries over many years without obvious warning? Fatty deposits, including cholesterol, gradually cling to inner vessel walls. Does that truly matter? Absolutely. Over time, those deposits harden into thick plaques—a process known as Atherosclerosis—causing once-flexible passageways to stiffen and narrow. Picture water forcing its way through an old, crusted garden hose; flow slows, and oxygen with vital nutrients struggles to reach tissues efficiently. As constriction progresses, resilience declines and risk steadily climbs. Concerning? Yes. Unchangeable? No. Early, consistent action through balanced nutrition, regular movement, and routine medical evaluations can slow plaque development, preserve circulation, and safeguard long-term vitality with steady confidence.
Have sudden, unfamiliar aches around temples ever sparked a quiet question—“Is this simply age catching up?” What if it signals something more? Giant Cell Arteritis often appears after fifty, quietly affecting arteries along head and neck. When those vessels become inflamed and narrow, vital nourishment to sensitive tissues can decline. Concerning? Yes. Hopeless? Absolutely not. Early recognition changes everything. Prompt medical evaluation and timely treatment sharply reduce risk of lasting harm. Strength lies in swift action. Confidence grows from awareness. Choosing to respond quickly protects vision, preserves independence, and keeps life moving forward with clarity and purpose.
Ever wonder what happens when relentless pounding inside arteries never truly eases? It may go unnoticed at first, yet over time that quiet force steadily wears structures down. Constant pressure pushes against delicate vessel walls, and little by little flexibility fades. Hard to see with bare eyes, isn’t it? Still, impact is real. As years move forward, those pathways grow stiffer and narrower, making blood flow less smooth where it matters most. When ongoing strain lingers, buildup begins to form, slowing circulation and raising serious risk. Concerning? Absolutely. Yet here is empowering truth: once awareness sets in, decisive steps can strengthen resilience, ease strain, and preserve vitality for many years ahead.
Diabetes: Elevated blood sugar levels over time can lead to damage in the vascular system, increasing the likelihood of complications.
Other Risk Factors: Smoking, high cholesterol, and a history of heart disease or stroke can also elevate the chances of developing this issue.
What Should You Do If You Think You’re Experiencing One?
If any of these symptoms occur—especially sudden vision loss—it’s essential to act quickly. This is a medical emergency, and prompt treatment can significantly help preserve sight.
Here’s what you should do:
Respond Without Delay
Even if that strange sensation flickers in and out or lasts only a heartbeat, isn’t it worth pausing to take it seriously? When surroundings turn fuzzy, dim, or briefly vanish, could that be an urgent signal asking for attention? Absolutely. Those shifts are not harmless quirks to dismiss after a long day—they often point to something deeper that feels unsettled. Why silence senses that clearly recognize change? Early awareness can prevent far greater difficulties later. Choosing to notice, to respond, and to move forward with purpose reflects strength and wisdom—and that decision can safeguard what matters most.
Sometimes, such disruptions appear without noticeable discomfort, making them easy to miss. Paying attention to subtle cues and acting promptly becomes crucial. Waiting or assuming conditions will resolve on their own can allow underlying issues to intensify, reducing ability to sustain regular routines and normal rhythm.
Why wait and keep guessing—why take that chance? Go to an emergency centre immediately or call for urgent assistance without delay. A thought may surface, “Is this an overreaction?” No, this is wisdom in motion. When vision shifts suddenly, swift action shows strength and awareness. Speak clearly about what changed—say, “Right side turned dark,” or “A shadow sits in center of vision and will not fade.” Clear words carry weight. Prompt, direct communication gives medical professionals precise details needed to respond without hesitation, and that decisive step can protect precious moments ahead.
Swift and accurate response can turn a moment of struggle into an experience that concludes effortlessly rather than stretching into a drawn-out ordeal. Hesitation or delay often allows small issues to expand into greater complications, while prompt action increases chances of restoring balance and preventing further difficulty.
When speaking with a medical expert, clarity can make a powerful difference. Why settle for vague phrases when precise words tell a stronger story? Describe exactly what is happening, when it began, how long it lasted, and whether it changed or stayed constant. Instead of saying, “Something feels off,” try clear statements such as, “Vision on left side went completely dark within seconds,” or “A misty, shadowed area remains in center of sight and has not faded for thirty minutes.” Notice how specific timing, location, and intensity create a sharper clinical picture. Did brightness shift? Did flashing lights appear? Did discomfort accompany visual change? Each detail adds valuable context. Clear, direct communication allows that expert to understand urgency, identify possible causes more efficiently, and move toward appropriate next steps without delay.
Long-Term Management and Recovery Oversight
Once that intense moment settles, does journey simply stop there? Of course not—temporary relief is only one step. What follows carries equal importance. Ongoing follow-up visits provide reassurance and sharpen awareness, catching subtle shifts that might otherwise pass unnoticed. A thought may arise, “Is it really necessary if everything feels fine?” Absolutely. Skilled specialists rely on advanced imaging and precise examination methods to evaluate delicate internal structures, detecting minor irregularities long before larger complications develop. Consistency builds protection. Each scheduled visit strengthens long-term stability, preserves clear function, and reinforces confidence in months and years ahead.
During every session, specialists perform thorough assessments using advanced imaging tools and precise diagnostic techniques to track changes in affected areas following earlier interventions. Past information undergoes close comparison to detect even minor shifts or signs of improvement. Findings may lead professionals to adjust previous approaches, test new strategies, or maintain careful observation through scheduled follow-up sessions.
Beyond technical aspects, ongoing visits create space to discuss any hurdles faced—such as trouble with reading, identifying familiar faces, or moving around different surroundings. Specialists can suggest tailored approaches, including custom lenses, adaptive tools, or small lifestyle adjustments that bring noticeable improvement in everyday living.
Maintaining consistent follow-up sessions goes beyond routine—it ensures early detection of hidden issues, careful tracking of progress, and a smoother recovery process. Missing these sessions is like fixing a leaky pipe without checking behind walls; what appears normal at first glance can conceal deeper problems quietly forming, eventually becoming far more difficult to address.

Treatment Options
What determines recovery? It often comes down to what triggered it and how quickly specialists step in. You might ask, “Is it too late to make a difference?” Not at all—acting fast can significantly improve what happens next. Full clarity may not always return, but timely intervention can strengthen results and protect what remains. So what might that involve? Let’s walk through options that professionals commonly use to move things in a better direction.
Easing Pressure from Within:
Ever sense that something inside feels off and quietly demands attention? A question may rise—“Can this truly be corrected?” Yes, it can. In certain urgent situations involving elevated pressure within the eye, specialists may apply carefully selected medicated drops or perform a brief outpatient procedure known as Anterior chamber paracentesis. During this precise step, a very small amount of fluid is gently removed from the front chamber of the eye, allowing internal pressure to decrease and delicate structures to stabilize. Sounds intense? In skilled hands, it is controlled, efficient, and purposefully designed to protect sensitive tissues while easing strain. Acting early and placing trust in experienced professionals greatly improves chances of restoring comfort, preserving vision, and regaining steady clarity.
Gentle Massage: In some cases, light pressure on the eye can help dislodge a clot and restore circulation.
Medications:
Have questions ever surfaced like, “Can a prescription truly change outcome?” Yes, it can. In urgent circulation events, medications such as Alteplase work by dissolving clots that obstruct critical blood flow, while anticoagulants like Heparin reduce further clot formation and keep movement smoother. When pathways reopen, oxygen and vital nutrients can once again reach tissues that depend on steady delivery to remain active and resilient. Powerful? Absolutely. Each therapy operates through a precise mechanism, targeting underlying blockage and restoring internal balance. Guided use under medical supervision offers a meaningful opportunity to safeguard function, reduce complications, and move ahead with renewed stability and confidence.
Oxygen Support via Concentrated Air:
Have thoughts ever drifted toward how something as simple as enriched air could create meaningful change? In certain urgent circumstances, clinicians administer concentrated oxygen through a fitted mask to elevate oxygen levels circulating in blood. Why does that matter? Because when circulation has been compromised, increasing available oxygen can enhance delivery to vulnerable tissues struggling from reduced flow. In some cases, advanced approaches like Hyperbaric oxygen therapy further amplify this effect by delivering oxygen under controlled pressure, improving diffusion into areas under strain. Reassuring? Absolutely. With stronger oxygen supply, cellular activity can stabilize, resilience may improve, and recovery gains momentum. When combined thoughtfully with other medical strategies, this supportive step can strengthen overall restoration and foster a steadier, more confident path forward.
Managing Conditions Linked to Internal Strain:
Maintaining control over concerns such as increased arterial pressure, fluctuating sugar balance, or long-lasting internal imbalances remains crucial for minimizing chances of future complications. Consistent routines, timely evaluations, and dedication to expert-directed plans foster stronger internal harmony. Through ongoing commitment and awareness, an individual can encourage smoother function, reduce strain on vital systems, and build greater resilience against severe outcomes that may arise later on.
Can It Be Prevented?
While complete prevention may not always be achievable, specific measures can reduce likelihood of occurrence. Adopting thoughtful daily routines, remaining physically active, and monitoring subtle warning signals can significantly enhance overall resilience and general well-being.
Keep your pressure levels steady by focusing on nutritious meals, staying physically engaged with regular movement, and following through with any treatments or prescriptions provided by your medical provider. Staying consistent in these areas helps support overall wellness and keeps your system functioning smoothly.
Managing Diabetes Effectively:
Managing diabetes demands steady focus and strong self-discipline. Keeping track of sugar levels comes first, since awareness makes it simpler to stay on course. Following an eating plan that maintains energy balance throughout each day adds stability. Taking prescribed medication exactly as advised and never missing a dose remains essential for consistency. Routine check-ins with medical professionals allow early spotting of any shifts that might need attention. Alongside this, staying active, practicing calming routines to ease tension, and making balanced lifestyle choices all combine to lower chances of future complications and keep overall wellness steady.
Quit Smoking: Impact on Circulation and Overall Wellness
Ever pause and ask what truly unfolds inside with every cigarette? Toxic chemicals do not vanish—they enter bloodstream, constrict delicate vessels, and limit steady delivery of oxygen and vital nutrients. Notice stamina slipping or fatigue appearing sooner than before? That connection is real. Continued smoking fuels inflammation, stiffens arteries, and accelerates processes like Atherosclerosis, placing added strain on heart and circulation. Harmless habit? Not at all. Yet here stands powerful truth: stopping changes trajectory. Within weeks, circulation begins to improve. Within months, lung function strengthens. Over time, cardiovascular risk declines significantly. Fresh oxygen flows more freely, endurance rises, and daily movement feels steadier. Worth reclaiming that vitality? Absolutely. Strength to choose differently already exists—and each smoke-free day builds measurable progress toward renewed energy and long-term resilience.
Keep Cholesterol in Check
Have thoughts ever turned to what quietly unfolds when cholesterol remains elevated for years? Fatty particles do not remain harmless—they gradually embed along inner arterial walls, thickening over time and contributing to Atherosclerosis. Notice breath shortening sooner than before or endurance dipping without clear reason? That cumulative strain is real. As vessels narrow, heart muscle must generate greater force to maintain steady circulation of oxygen and vital nutrients. Concerning? Certainly. Unchangeable? Not at all. Dietary patterns rich in whole grains, leafy greens, legumes, lean proteins, nuts, seeds, and heart-friendly oils can improve lipid balance. Regular movement enhances vascular flexibility. When appropriate, medications such as Atorvastatin reduce LDL levels and slow plaque progression. Consistency and professional guidance create measurable impact. With informed choices and steady commitment, cardiovascular performance can remain strong, resilient, and prepared for years ahead.
Maintain Regular Sessions: Meeting with a skilled professional consistently allows early detection of minor changes before they disrupt daily routines. These evaluations often uncover issues while still developing, creating more opportunities for effective management. Acting promptly helps preserve smooth coordination of all functions. Even when everything feels normal, sticking to routine assessments is a proactive and wise strategy.
Living with Vision Loss After a Stroke
Noticing a sudden change in how clearly surroundings appear can stir a mix of surprise and concern. Simple activities that once came naturally might now need extra focus, while daily habits may call for small adjustments to feel comfortable again. Even so, steady improvement remains achievable. With consistent effort, calm thinking, and practical methods, each step forward becomes more manageable. Below are several thoughtful ways to make this phase feel easier and bring back a stronger sense of assurance in everyday life:
Explore Useful Aids for Easier Day-to-Day Living:
When clarity begins to lessen or sharpness starts to wane, certain tools can truly transform routine activities. Items like magnifiers for reading fine print, glasses tailored for clearer sight, and screen readers that turn written words into spoken ones create smoother ways to manage regular tasks with less effort. From reading labels while shopping to browsing on a phone or finishing work on a computer, these resources make it easier to stay efficient and self-reliant. Each one aims to lessen frustration, preserve independence, and bring comfort back into daily routines.
Create a Safer Living Space: Brighten up each room with strong, consistent lighting to reduce shadows and dark corners. Clear pathways by moving furniture, cords, or loose rugs that could cause someone to stumble. Add bold, contrasting colors to items like stair edges, light switches, and countertops so they stand out clearly against their surroundings, making daily navigation much simpler and more secure.
Connect with Others: Sharing experiences with those who have faced similar challenges can provide significant comfort. Joining a group, speaking with a counselor, or opening up to a trusted companion allows for attentive listening and understanding. Major shifts in daily routines can feel overwhelming, but navigating them alone isn’t necessary. Supportive individuals can offer practical guidance, encouragement, and a reminder that you aren’t facing this journey in isolation.
Keep Moving Ahead: Life often takes unexpected turns, yet that doesn’t mean beloved hobbies or daily routines must disappear. With small adjustments and creative thinking, favorite activities can still be part of everyday life. Enjoy peaceful walks through open spaces, dive into captivating stories, nurture growing plants, or get creative with crafts and projects. Simple strategies and thoughtful tools can make these changes easier, allowing continued participation in what brings happiness. Staying engaged in meaningful pastimes lifts spirits, keeps thoughts clear, and adds a steady sense of fulfillment to each day.
Can it affect both eyes at once?
Have thoughts ever drifted to what it would mean if vision faded on both sides at once? That scenario is uncommon, yet when it occurs, urgency cannot be overstated. Why would such a change happen? Because oxygen and vital nutrients may no longer be reaching critical brain tissue as intended. Could arterial swelling or narrowing disrupt that flow? Absolutely. One serious cause is Giant Cell Arteritis, a condition affecting medium to large arteries—often near temples and jaw. When inflammation tightens those vessels, circulation drops and risk of permanent vision loss rises quickly. Alarming? Yes. Manageable with swift treatment? Also yes. Immediate medical evaluation, often followed by prompt corticosteroid therapy, can dramatically reduce complications. Taking sudden bilateral vision changes seriously and acting without delay can preserve sight, protect brain function, and prevent lasting harm.
When awareness of surroundings weakens on both sides, it often signals something more serious than a small, isolated concern. It can point toward involvement of a wider system that carries essential elements across an entire structure. Once that network falters, disruptions can spread across multiple areas. Such a moment calls for immediate attention. Acting fast by contacting a qualified professional or going straight to an urgent facility can change how events unfold. Rapid evaluation allows specialists to pinpoint causes, take corrective steps, and possibly stop further damage. Early response often improves chances for regaining function and limits long-term complications.
Can it cause long-term complications?
What unfolds when early warning signs are brushed aside? Subtle shifts rarely vanish on their own—they can settle in quietly and become harder to reverse. Notice surroundings losing sharpness or colors appearing less vivid than before? Catch a moment of squinting at text or hesitating when recognizing a familiar face? That is not imagination. Dim patches, faded areas, or small missing sections within a scene can signal reduced circulation to delicate retinal tissue, sometimes linked to conditions such as Retinal artery occlusion. Frustrating? Absolutely. Reading may demand greater effort, driving can feel uncertain, and steady footing might waver. Yet acceptance is not requirement. Early recognition paired with prompt medical evaluation offers a meaningful opportunity to preserve remaining vision, stabilize function, and maintain confidence moving forward.
What unfolds when steady nourishment to vision quietly declines over time? At first, changes may feel subtle—barely noticeable. Yet deep within retina, highly specialized light-sensing cells depend on constant oxygen and nutrient delivery to remain functional. When supply drops, resilience weakens. Could swelling or thinning gradually appear? Yes. Persistent deprivation can lead to structural breakdown, sometimes progressing toward conditions such as Retinal ischemia. In response, tissue may attempt compensation by forming fragile new vessels—a process known as Neovascularization. Reassuring at first glance? Perhaps. Stable solution? Unfortunately not. These newly formed vessels often lack durability, increasing risk of leakage, bleeding, or scarring that further compromises clarity. That is why early recognition and prompt medical evaluation carry such weight. Prevention and timely treatment preserve structure and function far more effectively than attempting reversal after significant injury has occurred.
Concerned that progression might continue? That feeling is understandable—and effective options exist. Consistent treatment truly changes outcomes. Specialists may recommend Laser photocoagulation to precisely target fragile or leaking vessels, sealing problem areas before further damage develops. Intimidating at first thought? In reality, it is carefully calibrated for accuracy and tissue protection.
In other cases, medications delivered through intravitreal injection—such as Ranibizumab—help reduce swelling, inhibit abnormal vessel growth, and stabilize retinal structure. Overwhelming initially? Perhaps. Purposeful and evidence-based? Absolutely. These therapies are designed to preserve remaining function and slow disease progression.
Commitment to a structured plan, regular monitoring, and collaboration with a retinal specialist transform uncertainty into direction. This approach is not passive reaction—it is deliberate action to safeguard vision and maintain long-term stability.
Long-term management often involves regular visits with specialists who keep a close watch and adjust plans when needed. Approaches may shift over time based on how someone responds or adapts to new methods. While a full reversal rarely happens, steady routines and proper techniques can preserve stability. With personalized exercises and ongoing expert guidance, many people continue daily activities with more ease, confidence, and control.
Can lifestyle adjustments truly cut chances of developing this condition?
Handling this condition over time often involves ongoing visits with professionals who monitor changes closely. Strategies may evolve as each individual responds differently. Though a complete reversal rarely occurs, consistent effort can maintain stability and allow a person to continue daily activities with confidence through well-chosen routines, exercises, and continuous direction from specialists.
Nourishing Meals for Everyday Energy: Designing meals with a vibrant variety of fruits, fresh vegetables, whole grains, and protein sources such as beans or fish can boost daily performance. These selections help maintain steady energy, promote smooth circulation, and support balanced digestion and metabolism. Following this approach consistently over weeks and months can improve management of sugar spikes, stress, and elevated pressure, fostering a sense of stability, endurance, and overall resilience day after day.
Regular Exercise: Why Staying Active Matters
Staying active on a regular basis keeps everything running smoothly. Movement helps circulation flow well, takes strain off heart function, and makes weight management easier. Consistent activity lowers chances of sluggish slowdowns that can sneak up over time. Whether it’s a walk around nearby streets, a bike ride in warm sunshine, or laps in a pool, frequent motion builds endurance, boosts stamina, and leaves you feeling energized and ready to take on days ahead.
Still thinking one cigarette barely matters? It matters more than imagined — and that truth deserves attention. Each spark sends harsh chemicals rushing through vital pathways, quietly tightening passages that carry oxygen and nourishment where life depends on flow. Notice subtle fatigue, shorter stamina, slower bounce-back? That isn’t coincidence. Damage builds silently, pressure rises, resilience fades. But what happens when a different choice is made? Strength starts rebuilding. Circulation improves. Breathing feels lighter. Movement feels freer. Confidence grows with every smoke-free hour. Difficult decision? Perhaps. Powerful turning point? Without question.
Ever whisper, “Everything’s under control,” while pressure keeps rising within? That tension doesn’t stay locked in thoughts; it travels deeper, stirring chemical changes that tighten vessels and urge heart to push harder than necessary. Feel that quiet fatigue, that subtle drain on momentum? Ongoing strain can slowly chip away at vitality and dim natural spark. Overwhelming? It doesn’t have to remain that way. When a pause is taken, when slow breaths expand chest, when muscles move with intention, when true rest becomes priority, balance begins to return. Mood steadies, circulation eases, inner strength rebuilds. More influence exists than first believed, and small daily shifts can restore calm, resilience, and lasting energy.
Carving out moments to relax isn’t merely a luxury—it plays a key role in overall balance. Focusing on slow, deliberate breaths can calm racing thoughts, while a peaceful stroll lets built-up stress slip away. Writing down reflections can untangle a cluttered mind, offering a sense of clarity. Gentle movements like yoga release tension from muscles and foster a feeling of lightness, and even taking a break from screens allows mental chatter to quiet, leaving space for calm and focus.
Spending a few peaceful minutes daily allows space for ease and clarity to settle in. Turning this into a steady practice brings a soothing pace, reduces unexpected spikes in pressure, and creates a sense of calm during regular checks. Gradually, it shifts from big changes to consistent, gentle actions that lighten strain across chest and thoughts, allowing each passing day to move with greater ease and balance.
Do lifestyle shifts truly change outcomes, or does doubt whisper that damage has already been done? Truth stands firm—power still exists. Adjustments may not erase every risk, yet steady choices can greatly lower chances of serious vascular complications. When balanced meals become routine, when daily movement stays consistent, when hydration remains steady, when stress is guided into calmer patterns, arteries grow stronger and circulation flows with greater ease. Notice how small actions repeated each day create meaningful momentum? Perfection isn’t requirement—consistency is. Stay consistent, and a lasting advantage begins to unfold, one intentional decision at a time.
Final Thoughts
Feels unsettling when sight shifts without warning, doesn’t it? Question arises, “Is this serious, or will clarity return on its own?” Deep down, awareness already answers—swift action changes everything. When vision blurs or something feels off, why leave it to chance? Quick response can safeguard what matters most. And what about days ahead? Choosing steady routines, staying active, tuning in to subtle signals—aren’t those powerful steps toward lowering future risk? Absolutely. Staying alert and proactive strengthens odds of continuing to see life with brightness and confidence for years to come.
Sight defines almost every moment—catching a smile from across a room, reading words that spark imagination, or watching sunlight dance on water. Many rarely pause to appreciate how much this sense contributes to daily living until something starts to change. Staying observant and tuned in plays a key role. When vision starts to act differently or feels uncertain, reaching out to a professional in visual wellness becomes essential. Taking timely action can prevent small concerns from turning into larger struggles and restore peace of mind for what lies ahead.



