Newborns’ Brachial Plexus Injury: Parent Guide
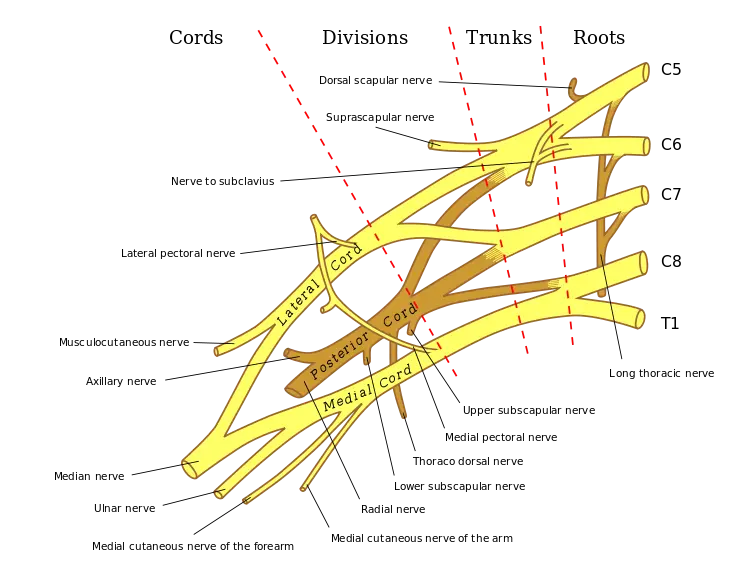
Picture this moment—you’re overflowing with happiness as your baby arrives, yet something feels off when one tiny arm stays limp. That stillness might point to a nerve concern affecting movement through shoulder, arm, or hand. Such situations can occur during birth, particularly when delivery is complicated or when babies are larger in size. Although rare—appearing in about one to three out of every thousand births—many parents have faced similar challenges. Reaching out to a doctor can provide direction and reassurance so your little one gains strength and continues to grow with ease and confidence.
There are four main types of injuries in newborns:
| Type of Injury | Description |
| Neuropraxia | Mildest form; temporary conduction block due to myelin sheath damage |
| Axonotmesis | More severe; nerve fibers disrupted but myelin sheath intact |
| Neurotmesis | Most severe form, involving complete disconnect that requires rebuilding function entirely from scratch. |
| Erb’s Palsy (C5-C6) | Upper plexus injury; affects shoulder and elbow flexion |
| Klumpke’s Palsy (C8-T1) | Lower plexus injury; affects wrist and hand function |
| Total Plexus Palsy (C5-T1) | All nerves involved, resulting in total paralysis of arm |
Neurapraxia is considered the most frequent type of nerve injury, where fibers are stretched yet remain undamaged. This condition usually results in temporary loss of movement or sensation, but natural healing tends to occur over time. Most infants experiencing it regain full function within several weeks or a few months as normal nerve activity gradually returns.
In contrast, Neurotmesis represents a far more serious situation. It happens when nerve fibers are completely torn apart, cutting off communication between muscles and the brain. Recovery from this stage can be difficult, and in some cases, improvement may be only partial or might not occur at all, even with consistent therapy.
Avulsion represents an even more severe condition, marked by full separation of nerve roots from spinal region. Once this type of injury occurs, return of normal motion is highly uncommon, as signal transmission pathways have been completely disrupted.
Another condition involves a lower section of that nerve network near the spine, often seen during breech births. Infants experiencing this may display noticeable weakness or restricted motion in one lower limb, sometimes showing imbalance or reduced coordination on that side.
| Type of Injury | Prognosis |
| Neuropraxia | Most recover fully within 3 months |
| Axonotmesis | Often recovers within months, but may not be complete |
| Neurotmesis | Recovery possible, but often requires surgery and extensive therapy |
| Erb’s Palsy (C5-C6) | Good prognosis, often recovers within 6 months |
| Klumpke’s Palsy (C8-T1) | More challenging prognosis, may require long-term therapy |
| Total Plexus Palsy (C5-T1) | Variable prognosis, depends on severity and treatment |
Main cause in infants often involves excessive pulling or twisting near neck area during delivery. Chances increase when newborn is larger in size, maternal pelvis is narrow, or birthing process becomes prolonged or complicated.
Additional potential causes:
Shoulder dystocia:
This occurs when a baby’s shoulder becomes stuck behind a parent’s pelvic bone during birth.
Forceps delivery is occasionally used when extra guidance is needed during childbirth. These metal instruments are placed around an infant’s head to assist in guiding the baby out safely. When handled with precise skill, they can make delivery smoother, especially in challenging situations. However, if applied with excessive pressure or positioned incorrectly, nearby nerves and soft tissues can experience strain or injury. Such strain may lead to reduced sensation or limited movement in an infant’s upper limb. In mild cases, normal motion usually returns over time, while more serious situations may result in longer recovery or partial restriction of arm function depending on how much pressure was applied during delivery.
Vacuum extraction is sometimes used during childbirth to guide an infant through final delivery stages. This technique uses a soft suction cup placed on an infant’s head to create gentle traction that aids movement through the birth canal. When positioned accurately and managed with care, it often allows a smoother delivery. If placement is off or excessive force is applied, delicate tissues and nerves may experience strain or injury. Such strain can cause difficulties with movement or coordination after birth. In mild situations, recovery usually happens gradually, while severe cases may bring lasting challenges with motion or muscle control based on how much pressure occurred during delivery.
If a little one experiences NBPP, it’s important to remember that many families have walked a similar path. Guidance and information are available from various professionals and community programs focused on improving movement and strength. A medical specialist can connect parents with experienced therapists and rehabilitation teams who design personalized exercises to encourage progress. With consistent care, patience, and encouragement, many children gradually regain movement and build confidence as they grow stronger and more independent over time.
In the interim, there are several proactive measures you can take to aid your baby dealing with NBPP:
- Cultivate patience and surround that little one with plenty of love, as recovery for most NBPP cases unfolds gradually through steady progress over time.
- Learn gentle positioning techniques for a little one to maintain flexibility and prevent stiffness or joint restriction.
- Get involved in gentle exercises with your baby, keeping your sights on preserving range of motion and building up strength.
- Keep a little one engaged by talking often and gently including that affected side during play activities. Simple games, songs, or reaching exercises can stimulate movement and coordination. Encouraging small actions like touching toys, clapping, or grasping objects helps build strength and awareness. Making these moments fun and interactive not only boosts physical development but also strengthens emotional connection, creating a positive space for steady growth and improved motion over time.
- Link up with other folks dealing with the same hurdles by joining a support group dedicated to NBPP.
Always remember, your little one’s got grit and toughness. With your steady love and backing, they got the chops to flourish, even with NBPP.

When your little one experiences trouble right after birth, you might notice something’s off right away—or it may take a little time to show. How things unfold depends on what’s been impacted and just how deep the issue runs.
Look out for these common signs:
- Lack of strength or movement in that side or hand.
- Reduced motion or sensation on that side.
- That side showing limited motion may appear slightly different or rest in an unusual position.
- Difficulty moving fingers or thumb
- No Moro reflex on one side (this reflex is when your little one stretches their limbs out wide and then pulls them back in).
Doctors often identify this condition in a newborn through a detailed physical check and review of medical history. In some cases, additional imaging such as X-rays, ultrasounds, or MRIs may be recommended to confirm details and determine extent of nerve involvement.
| Symptom | Description |
| Limited movement or strength on one side. | This can affect how efficiently certain muscles function, depending on severity and location of the issue. Common signs include: |
| * Erb’s palsy: Arm hangs limp, inability to raise arm above shoulder, weak grip. | |
| * Klumpke’s palsy: Claw hand, weak wrist and finger flexion. | |
| Total brachial plexus condition: Complete loss of motion and feeling throughout the entire upper limb. | |
| Reduced motion or sensitivity in an upper limb | This may vary from slight tingling to total loss of feeling, depending on which nerves are involved. |
| Unusual Placement of That Side | That side showing limited movement may stay fixed in one position, often with elbow bent and arm held close, or it might hang loosely without much control or response. |
| Missing Moro reflex on affected side | Moro reflex acts as a natural startle response where a little one spreads arms wide. When this reaction appears on only one side, it can suggest an issue affecting that particular area. |
| Decreased grip on the affected side | An infant may show a weak grasp or be unable to hold objects altogether. |
| Pain (less common in newborns) | Though uncommon in newborns, some may experience discomfort on that side or near shoulder region. |
Long-Term Challenges a Kid Might Face After This Kind of Setback
| Challenge | Description |
| Upper Limb Weakness | Hard time using that side because the muscles aren’t as strong as they should be. |
| Pain and Spasticity | Ongoing soreness and tight muscles in that side can make everyday movement tough. |
| Sensory Loss | Less or no feeling in that side. |
| Joint Deformities | Tightness or joint shifts may occur in that area, making movement increasingly difficult over time. |
| Psychological Impact | Emotional ups and downs, along with social challenges that arise after an experience like this, can place a heavy strain on an individual. |
When something feels off with a little one’s movement, what happens next depends on how serious things are and which areas are involved. In many cases, gentle motion exercises and everyday skill practice become part of recovery. One method focuses on improving coordination and flexibility through guided activity, while another teaches families to include that side naturally during feeding, dressing, or playtime. Combining both methods encourages steady progress, allowing a child to grow more confident and capable as strength and motion gradually return.
For less severe cases, non-surgical approaches take precedence, encompassing:
Physical Therapy: A physical therapist guides parents in gentle movement exercises for an infant’s affected arm and hand, reducing stiffness and contractures while encouraging steady flexibility and comfort.
Occupational Therapy: Occupational therapists guide families in including an affected limb during daily routines like eating and dressing, encouraging natural use and improved coordination over time.
Splinting or Casting: Use of splints or casts maintains affected arm in a position that promotes proper healing and reduces strain throughout recovery.
Medication: Use of prescribed medication to ease any discomfort an infant might experience during recovery.
In more serious situations, surgery may become an option, often considered when a child is between three and six months old. This procedure focuses on repairing damaged nerves or transferring muscles from one area to another to restore movement and strength. The main goal is to improve overall function and create the best possible path toward recovery, giving that little one a stronger chance to move, play, and grow with greater ease and confidence.
| Treatment | Advantages |
| Non-operative Management | – Minimally invasive – Gives the body a chance to bounce back naturally on its own – Lower risk of complications |
| Nerve Grafting | – Improves functional outcomes for severe injuries – Can restore sensation and function |
| Neurolysis | – Relieves pressure on the affected area, allowing it to function more efficiently again. – Can restore movement and sensation more effectively. |
| Muscle Transfers | – Provides alternative function for paralyzed muscles – Improves quality of life |
After the Operation: Once it’s all done, your little one will need some gentle guidance to get things moving again and build up strength on that side. Getting back to the swing of things might take a few months—or maybe a bit longer. But hang in there. With steady encouragement and plenty of love, most kiddos bounce back and go on to enjoy active, happy lives.
What lies ahead for little ones in this situation? Honestly, it comes down to how much was impacted and exactly where. Many bounce back just fine over time, but for some, there may be lingering struggles with movement or strength on one side.
Financial Assistance and Insurance Guidance
Raising a little one with this kind of challenge takes patience, strength, and a whole lot of heart. Even when the days feel long or uncertain, just remember—they need your steady love more than anything. Here are some down-to-earth tips to help guide you through:
Hang in there—healing from this type of nerve damage takes time. Stay positive, and don’t get discouraged if progress isn’t immediate.
Show Extra Love: Pour on the hugs and reassurance during this important time. Let your little one know you’re right there beside them and believe in their ability to push through whatever comes their way.
Acknowledge Incremental Progress: Acknowledge every bit of progress, no matter how small. Celebrating these moments builds motivation and boosts confidence, encouraging a child to keep trying. Consistent recognition of effort nurtures determination and creates a positive mindset that turns each step forward into a meaningful achievement.
Reach Out for Help: Take advantage of every resource available for parents facing this challenge. Talk to your doctor about finding support groups or online communities where you can connect with others who’ve been in your shoes.
Find Your Circle: Remember, this journey isn’t one you’re taking alone. Connect with parents and families who’ve faced similar experiences—they understand every high and low. Sharing stories, advice, and encouragement can bring comfort and strength. With patience, compassion, and good people around you, both you and your little one can overcome challenges, celebrate progress, and keep finding joy in everyday moments.
Collaborate with medical professionals caring for your child. Consistent communication and shared planning make it easier to address challenges directly and create strategies that promote steady growth, comfort, and overall well-being. Working as one team ensures your child receives the best possible care and encouragement throughout recovery and development.
Author Bio:
Pamela Harris is an experienced medical writer collaborating with US Health Hub. Her focus lies in providing parents with clear, practical insights into infant wellness topics. With a talent for simplifying complex information, Pamela ensures families can easily understand important details and feel confident navigating challenges related to their little ones’ growth and well-being.



