Ischemic Stroke & CT Scans: A Quick Guide
During critical medical emergencies, speed decides outcomes. Each second matters, and fast recognition plus immediate action improves results. One form appears far more often than all remaining types, reaching almost 87 percent of cases. Knowing what sets it off, how it unfolds, and how clinicians spot it so fast matters. A major tool here is a CT scan, offering rapid, detailed views inside. By looking at causes, underlying processes, and diagnostic methods, readers see why this imaging option often proves central during urgent moments.
What Is an Ischemic Stroke?
This condition happens when blood flow to a specific part of brain becomes blocked or significantly reduced. Without oxygen and essential nutrients, brain cells start dying within minutes. Picture it as a severe traffic jam in vessels supplying brain tissue. If blockage isn’t resolved quickly, damage can become permanent, causing long-term disability or even death.
Most cases result from formation of a blood clot. Clots can form directly inside brain arteries or travel from other areas, such as heart, before lodging in a vessel. Risk factors that increase chances include high blood pressure, elevated cholesterol, smoking, diabetes, and irregular heartbeat, such as atrial fibrillation.
Why Early Diagnosis Is Critical
Brain tissue is extremely sensitive. Without oxygen, cells start dying at an estimated rate of 1.9 million per minute. Every second counts when this type of emergency happens. Rapid recognition and timely intervention significantly improve chances of limiting damage and achieving better recovery.
Imaging holds a vital role during urgent moments. Clinicians often choose it as first diagnostic step since scans run fast, stay broadly accessible, and deliver dependable insight for spotting urgent issues that disrupt brain function.
What Is a CT Scan?
An advanced X-ray–based approach captures highly refined internal visuals by rotating around a person and collecting multiple views from varied angles. Unlike basic X-ray imaging that creates a flat, single-layer picture, this approach assembles dozens or even hundreds of slices to form a complete three-dimensional view. Such layered perspective gives clearer insight into ongoing changes, especially during moments when time matters most.
When someone suddenly collapses, struggles to speak, or shows unusual facial muscle movement, this scanning method becomes extremely valuable. It can detect whether a major vessel supplying oxygen is blocked or if bleeding has occurred due to a ruptured vessel. Outward signs may appear similar, yet each situation requires completely different steps to stabilize the person.
By delivering rapid, high-resolution results, this scan allows specialists to distinguish between these serious internal problems within minutes. Speed is critical, as central control center of brain—responsible for memory, movement, and vital functions—can begin sustaining permanent damage if wrong condition is treated or intervention is delayed.
This advanced X-ray technique is often first step in emergencies because it works quickly, provides detailed visual information, and allows specialists to understand what is happening inside head. Images reveal blockages, swelling, or other urgent changes, enabling immediate decisions about necessary actions.
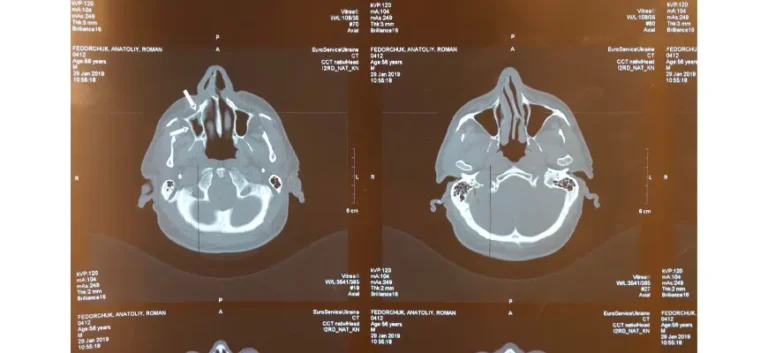
How does it work for diagnosis?
When someone shows sudden weakness along one side, slurred speech, or facial drooping, staff react at once with urgency. One early step uses a high-speed internal head scan that works without injected contrast agents.
Preparation: Individuals rest on a motorized platform that moves gently into a tunnel-shaped machine resembling a large doughnut. No needles or incisions take part, keeping experience smooth and comfortable. Some may feel mild confinement, especially if sensitive to enclosed spaces; slow, steady breathing and closed eyes often ease tension.
Scanning: Machine rotates gently around head, capturing a series of X-ray images from multiple angles. Process usually finishes within a few minutes, producing a clear internal view of head structures.
Image Reconstruction: Once data is collected, a computer combines images from different angles into highly detailed, layered visuals. Cross-sectional views reveal subtle abnormalities such as swelling, unusual darkened areas, or tissue changes, allowing experts to understand whether a serious issue is affecting central nervous system function.
Interpretation: Trained specialists review visuals closely to determine if an event has occurred and identify its specific type. Insights from this review guide immediate actions, whether that involves medication, a procedure, or other measures needed to stabilize an individual.
Fast, non-invasive scanning is crucial in time-sensitive emergencies, providing clear, immediate insight so response teams can act efficiently and confidently.
What Can It Detect If Someone Has a Brain Blood Flow Problem?
In early stages, imaging may appear normal because changes within brain tissue can be very subtle. Specialists look for specific indicators, including:
Loss of Gray-White Differentiation: Normally, soft tissue regions responsible for processing signals and those handling transmission show clear contrast in internal visual assessments. When sudden disruption occurs within central nervous system, this contrast can fade or vanish in affected areas, making it harder to distinguish between these critical tissue types.
Hypodensity: This describes darker regions on internal visuals, often suggesting that an area is not receiving sufficient oxygen or nutrients. Shadowed zones may indicate early tissue injury, where cells struggle to function properly due to reduced circulation.
Sulcal Effacement: Natural grooves and folds on central nervous system surface, known as sulci, can sometimes appear less defined or seem to disappear in certain internal visuals. This usually happens when internal pressure increases, often caused by swelling in surrounding tissue. Expanding tissue compresses grooves, making them harder to see on diagnostic images.
Hyperdense Artery Sign: When an obstruction occurs in a main circulation pathway inside the head, it may appear as an unusually bright area on specialized internal scans. This bright signal often indicates a clot lodged within a vessel, restricting normal flow through that channel.
Even though these indicators can be subtle, experienced specialists can often identify them during early stages, allowing timely action to address potential problems.
Why Is It the First Choice for Stroke Diagnosis?
Several factors make this imaging tool a top choice for diagnosing it:
Speed: In emergencies, acting quickly can be life-saving. One major advantage of this scan is its rapid execution. A basic version—without contrast material—can often be completed within minutes. Such quick results allow teams to assess a situation immediately and determine next steps without delay.
Accessibility: This technology is widely available in facilities of all sizes, from large urban hospitals to smaller community clinics. Its broad presence ensures individuals in both cities and remote areas can receive timely evaluation when urgent neurological issues arise.
Precision: While very early signs might not always appear, this scan is highly reliable for detecting internal bleeding. This distinction is critical because different actions are required depending on underlying causes.
Safety: This procedure is generally considered low-risk, though it involves minimal radiation exposure. In urgent scenarios, gaining a rapid understanding of internal conditions often outweighs concerns about radiation. Many find that clarity and speed provided by this method make it an effective first step in urgent situations.

Limitations of Brain Imaging in Diagnosis
While highly valuable, this imaging approach has some limitations, especially for detecting very early strokes. During first hours, changes within brain tissue may be too subtle to appear clearly. For this reason, specialists often rely on additional tests, such as MRI scans, to confirm a diagnosis or assess full extent of damage.
MRI technology can show subtle internal changes far earlier than traditional scans. Still, process takes longer and may not always be accessible during urgent moments. In many situations, faster scanning happens first, with MRI added later once clinicians need deeper detail.
What Should You Expect After Getting Your Imaging Test Back?
Once results confirm an issue, immediate action aims to reopen pathways that deliver oxygen plus nutrients to affected regions. Several advanced options exist, based on severity plus timing. One option relies on specialized medication designed to dissolve obstructions and restore circulation. When this option proves unsuitable or ineffective, clinicians may choose a minimally invasive procedure. During it, a tiny device travels through vessels to physically extract blockage. Added steps often follow to control internal pressure, steady someone involved, plus lower chances of repeat events.
Thrombolytic Therapy: Often called “clot-busting” medication, agents like alteplase (tPA) act by breaking apart obstructions that block oxygen plus nutrients from reaching vital areas of central nervous system. When given soon after symptoms begin—usually within a very narrow window—these drugs can reopen affected vessels and limit added damage to nearby tissue. Timing matters greatly, since benefit drops sharply as obstruction stays in place longer.
Mechanical Thrombectomy: In certain emergencies, specialists may use a minimally invasive technique where a thin, flexible tube is threaded through vessel networks to reach blocked areas. Once there, specialized tools extract obstructions directly. This method is usually reserved for severe blockages or situations where clot-dissolving medications have not produced desired results.
Additional Measures: Medications may be given to manage internal pressure, especially within circulatory pathways, maintaining safe balance and reducing chances of new blockages forming in critical vessels. Other interventions may be applied to reduce swelling in central control regions, helping preserve vital functions and minimize long-term damage.
How Advanced Imaging Could Change the Way We Treat Brain Emergencies
Technological advances are making imaging increasingly powerful for diagnosing it. Perfusion imaging, for example, measures blood flow within brain tissue, helping specialists identify areas at risk of damage. Angiography using contrast dye visualizes vessels and detects blockages. These techniques provide highly detailed information, allowing for more precise and effective interventions.
Artificial intelligence (AI) is becoming an important tool for urgent neurological events. These smart systems can analyze advanced visual data in seconds, detecting critical internal changes with remarkable accuracy. In areas where expert interpretation may not be immediately available, AI can act as an additional layer, spotting early signs that could otherwise be missed. This emerging technology is transforming rapid decision-making, offering faster, more reliable assessment of internal conditions and guiding next steps efficiently.
Can it detect all types of ischemic strokes?
No, this scan may not detect every case, particularly during early stages. While a non-contrast version is highly effective at ruling out bleeding events, it may not always reveal an acute occurrence immediately. In certain situations, additional imaging such as CTA, CTP, or MRI is required for a more detailed evaluation.
How long does it take for stroke-related changes to appear on a CT scan?
Related changes may need several hours before becoming visible on a standard non-contrast scan. During first few hours after onset, results may still appear normal. However, subtle early signs like loss of gray-white matter differentiation, sulcal effacement, or hyperdense artery signs may be present. More advanced imaging techniques such as CT perfusion can help detect changes sooner.
Can it predict recovery outcomes?
A CT scan alone cannot accurately predict recovery, but it provides insight into extent of brain damage. Factors such as size and location of infarct, presence of swelling, and blood flow status from CT angiography or perfusion imaging offer valuable information. Recovery also depends on individual factors such as age, overall condition, rehabilitation progress, and speed of intervention.
Conclusion
This qualifies as a critical emergency where time decides outcomes. Advanced technology captures internal visuals with remarkable detail, allowing specialists to act fast and understand what happens inside head. Rapid response can separate a return to normal life from long-term complications. While these tools may miss some early signs, speed, broad access, and strong precision make them essential during urgent neurological events.
If someone shows warning signs—such as sudden weakness, confusion, or difficulty speaking—call 911 immediately. Every second matters, and fast action increases chances of full recovery. Cutting-edge imaging provides a quick, painless way to see inside head, giving specialists clear information for timely decisions and showing how far modern medicine has advanced.



